Cancer’s Community Drama: The Tumor Microenvironment Explained
Cancer isn’t just a collection of rebellious cells—it’s a full-blown ecosystem. The tumor microenvironment (TME) is the chaotic community where cancer cells thrive, manipulate their neighbors, and plot their next move to create more trouble. Understanding the TME is a game-changer for cancer treatment. It explains why some tumors grow fast, spread quickly, or resist therapy—and it’s helping researchers uncover new ways to stop cancer in its tracks. Let’s take a closer look.
What It Is
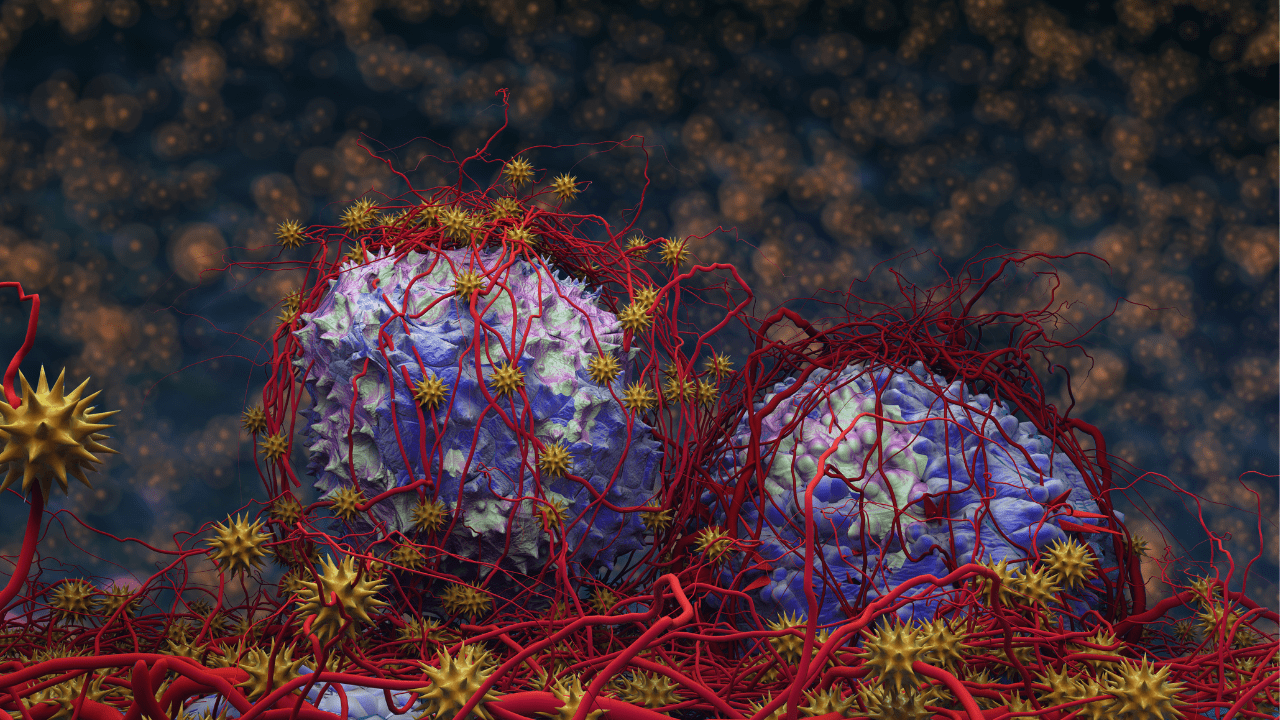
Think of the tumor microenvironment as cancer’s neighborhood. It’s not just made up of tumor cells, but also includes:
- Blood vessels: Delivering oxygen and nutrients to fuel tumor growth.
- Immune cells: Some fight the tumor; others get tricked into helping it.
- Fibroblasts: A type of cell gone rogue, laying down structural support for cancer.
- Extracellular matrix (ECM): The name given to the scaffolding that fibroblasts lay down, which can either block or promote cancer invasion.
- Signaling molecules: Act like text messages between cells, telling cells what to do.
This isn’t a quiet county village—it’s more like a bustling city with crooked cops, bribed officials, and a whole lot of noise.
Zoom In: Trouble Starts Early
In many cancers, the TME goes off the rails before a full tumor forms.
- Inflammation in the tissue? That’s like an open call for cancer cells.
- Fibroblasts laying down extra ECM? That’s a highway for tumor invasion.
- Immune cells confused by signaling molecules? That’s a security system turned inside out.
The result: a cozy, supportive cancer environment where tumor cells can grow, mutate, and dodge the body’s defense systems.
Zoom Out: Big Deal for Therapies
Cancer treatments used to focus mainly on killing tumor cells, but that’s only half the story. Targeting the TME opens up new options. For example:
- Anti-angiogenesis drugs block the tumor’s blood supply.
- Immunotherapies retrain immune cells to recognize and fight cancer.
- TME-modulating agents aim to break down the tumor’s support system.
Understanding the TME also helps explain why some tumors resist treatment—it’s not just the cancer cells, but their entire neighborhood working against you.
How It Works
- Blocking a tumor’s blood supply: Bevacizumab (Avastin, made by Genentech/Roche) is a monoclonal antibody that blocks VEGF, a key protein that tumors use to grow new blood vessels. Without fuel, there is no growth.
- Recognizing tumors: Pembrolizumab (Keytruda, made by Merck & Co.) is an immune checkpoint inhibitor that blocks the PD-1 pathway, helping T-cells recognize and attack cancer cells. It’s widely used across multiple cancers, from melanoma to lung and bladder cancer.
- Breaking down a tumor’s support system: Nivolumab (Opdivo, made by Bristol Myers Squibb) is a monoclonal antibody that blocks PD-1, helping T-cells stay active and attack cancer cells. Ipilimumab (Yervoy, also made by Bristol Myers Squibb) targets a different immune checkpoint called CTLA-4 to amplify the T-cell response further. Together, they’re a powerful one-two punch in cancer immunotherapy.
The Bottom Line
Cancer doesn’t grow alone—it needs a willing neighborhood. The tumor microenvironment shapes how cancer behaves, spreads, and responds to treatment. The more we understand this microscopic cityscape, the wiser we can be about evicting cancer from the body.
BioBasics 101 Live
Do you need a better understanding of biotechnology to engage with colleagues, clients, and investors? Join us May 20-21 in Seattle, Washington, for our most popular 2-day course: BioBasics 101: The Biology of Biotech for the Non-Scientist. Click here for more information.









